Frequent reports that the University College Hospital (UCH) Ibadan is under a spell of darkness and water shortage belie its pedigree as a top-notch medical centre for the training of doctors, healthcare delivery and research. But the fetid narrative perfectly reflects the lack of serious attention to the health sector, and life itself, in Nigeria.
The hospital’s pathetic condition has sparked countless protestations from a broad spectrum of its stakeholders and nostalgic feelings about the days of yore, when it was the flagship in healthcare delivery, not just in Nigeria, but in the whole of Africa. Therefore, the authorities in Abuja, and within the institution, should wake up to their responsibilities and buck this ugly trend.
For too long, this premier tertiary hospital established in 1957, has been, as it were, on a sick bed waiting for the surgeon’s blade. Its medical infrastructure is no longer cutting edge, and neither are its health services of high quality. However, its current exposure to public glare stems from the Ibadan Electricity Distribution Company‘s (IBEDC) decision to disconnect it from its services following a huge indebtedness of over N400 million as of April. By March, it had reportedly suffered three sustained blackouts.

The hospital’s Public Relations Officer, Funmi Adetuyibi, claims that there have been mitigatory responses in terms of providing measured electricity supply with its generating sets to some critical units like Emergency Departments, Intensive Care Units, Laboratories and Surgical Theatres.
But plaintive testimonies of the power supply reality by many relatives of the hospital’s patients brutally invalidate Adetuyibi’s PR stunts. One countervail puts it thus, “We are witnessing our loved ones suffer needlessly. Patients are dying because they cannot receive the medical tests required for treatment. These power outages have not only hampered immediate medical assessments but have gravely complicated ongoing treatments, leaving families in profound despair.”
This seeming vinegar is not swallowed by all patients, or their relatives, which has prompted some, who can afford to do so, to dejectedly leave the hospital to seek therapy elsewhere. It means doubling costs of treatment, amid inflationary pressures on Nigerians.
All the hospital’s stakeholders are bristling for protest or strike, in one way or the other, to instigate action. Leading the charge are the Joint Health Sector Union (JOHESU) and the Joint Action Committee (JAC) – the umbrella unions of health workers. The latter had rattled the UCH management in April with its resolve to work only from 8 a.m. to 4 p.m. daily, which invariably meant shunning night duties. The threat was so real that the hospital’s management issued a statement to warn the workers, including medical doctors, that “whoever fails to report at his or her duty posts does that at his own or her own risk.”
The UCH reportedly collects N14 million every month as its overhead cost from the Federal Government. But its monthly electricity bill is about N99 million. In this era of suspect classification of the hospital as Band A consumer, paying up under this energy supply structure is impossible.
Water is basic to human existence, more so in a hospital setting to stave off likely epidemics from a compromised environment. The groans of student-doctors on its shortage are loud and clear. Some wake up early in the morning to queue for hours to get it.
A recent statement from the hospital said its IBEDC bills, including accumulated arrears since 2019, amount to N3.1 billion. The outstanding bill is N400 million, just as “alternative power supply in solar panels and inverters have been deployed.” In a sharp contrast, “efforts to secure alternative energy provision are at advanced stage,” is another message from the same hospital. Nobody is in doubt, therefore, that the management is waffling about the matter.
It is beyond debate that the hospital is underfunded, just like similar institutions. In all of this grimy narrative, the hospital’s internally generated revenue is not publicly known. For the records, UCH has about 10,000 in-patients and 14,000 out-patients yearly. As a referral or specialist hospital not run on charity, it is our conviction that it should be able to generate some revenue to take care of its basic needs, where the government irresponsibly defaults.
But it has failed in this regard, having allowed itself to be gripped by the fabled incubus of government agencies that generate revenue but are unable to be self-sustainable. In sane jurisdictions, a hospital of UCH’s category should not be mired in this vortex it has found itself. There are private universities with teaching hospitals having world class equipment, funded only by their proprietors and businesses established to keep their operations going.
The UCH star should not be allowed to dim any further. But its sullied reputation as a teaching hospital of note, with dilapidated infrastructure and the mass exodus of its Consultants and other health professionals to Europe and the US in search of greener pastures, precedes the current debacle. The rot dates back to the mid-1980s when the economy came into a major tailspin, induced by Ibrahim Babangida’s Structural Adjustment Programme (SAP).
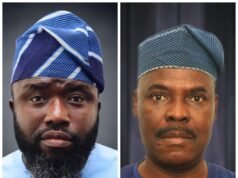
In his corroboration of the state of affairs, a former Chief Medical Director (CMD) of the institution, Professor Emitope Alonge, said, “Unfortunately, there was this issue of brain-drain syndrome. The bad economic situation forced many dedicated medical officers to emigrate in search of greener pastures. UCH felt it more… that was the beginning of the problem in the health sector in Nigeria, and at the UCH in particular.”
“There were so many things going on wrong at the UCH. There was poor power supply, operations were cancelled, no equipment, instruments and operating gowns were sterilised outside of the hospital, (and) there were cases on (of) infections and wounds.” Even its water was not silted.
Longe, who was a clinical student of the hospital between 1980 and 1983, added that when he came back from his medical training abroad in 1995, “that was probably, the peak of the disaster. People did what they liked; they had no culture. UCH has a culture that I knew we needed to try to infuse that culture into people. So, I was burdened about the decadence.”
It is incredible that a hospital of UCH standing only got a Molecular Laboratory in 2020, during to the global COVID-19 pandemic. A year before, it acquired its first Cardiographic machine. In fact, efforts to revamp it and restore its past glory have been few and far between.
As a result, the authorities of UCH, and by inference, the University of Ibadan, should think out of the box, and pull the hospital out of its present quagmire. Solar energy, an alternative electricity supply, should be embraced and sourced by the relevant departments in UI. Electricity bills are exploitative and the high cost of diesel used to power generating sets should be off their table. A company is harvesting solar energy from the Sahara desert to power the UK. This is a natural resource being wasted in Nigeria.
Therefore, setting up Centres for Energy Research and Development in our universities for solutions to national challenges such as that of UCH, has become imperative. At the University of Nigeria, Nsukka, for instance, the CERD was set up in 1982 while Professor Alexander Animalu chaired its Physics Department, and it enabled the institution to provide a solar energy system for its data centre, which is independent of the national grid; and it equally stabilised internet services within the university community.
In October 2021, about 600 doctors and other health workers resigned. Another of its CMD, Professor Abiodun Otegbayo, said he signed 15 resignation letters each week. Many of its specialists who are still in service have one leg already abroad, as is the case in the Obstetrics and Gynaecology department, where Dr Gholahan Obajimi disclosed that there are 11 Senior Registrars, and almost all of them have applied for training in the United Kingdom. “We certainly cannot influence people’s choices; everybody is free to live in any part of the world,” Obajimi noted, matter-of-factly. Many now go for training but hardly return.
The UCH must be made to recover its groove, which made it a hospital of first choice for members of the Royal family of the oil-rich Saudi Arabia in the 1960s and ranked the fourth best in the Commonwealth then. However, the truth is that this can only happen if President Bola Tinubu’s administration stops its binge of misplaced priorities. The N15 trillion 700-kilometre Lagos–Calabar coastal Highway and Sokoto to Badagry coastal highway – which is longer than the former and which has also been commissioned – provide pungent contexts of this.

Our public hospitals cannot be “mere consulting clinics” or human abattoirs, while the country under Tinubu’s leadership, commits a borrowed $350 million to the Kano – Marada (Niger Republic) railway project, which is of no immediate benefit to the country. His predecessor, Muhammadu Buhari, had expended a whopping $1.9 billion on the project already.
Nigeria urgently needs hospitals of global repute that could help in the drastic reduction of its medical tourism to Europe, USA and other regions, which gulps between $1.5 billion and $2 billion annually, according to a study in 2023.